Endometriosis Specialist - Denver, CO
Approximately 1 in 10 women will struggle with endometriosis pain during their lifetime. Fortunately, there are multiple treatment options for this painful condition.
Many women are told they must have a surgery to diagnose endometriosis. Although true it is more reasonable to initiate medical management on the assumption a woman has endometriosis.
At the Advanced Women’s Health Institute, we’re committed to providing you with the least-invasive options available We’ll listen and work with you to develop a personalized treatment plan that works for you.
If you’re ready to develop your endometriosis treatment plan, schedule an appointment with us today.
FAQs on Endometriosis
What is endometriosis?
When tissue implants are found outside of the uterus that look like your uterine lining, or endometrium, under the microscope we call this condition endometriosis. Implants of endometriosis are most commonly found in the pelvic area and on the ovaries, fallopian tubes, rectum and bladder dome. There are uncommon reports of endometriosis outside the pelvis such as in the lung, colon, inside the bladder, and even as far away as the brain.
What is an endometrioma?
Endometrioma is when endometriosis causes a cyst in the ovary. As endometriomas grow pelvic pain worsens, which frequently leads to surgery. Simply draining the cyst is ineffective as it will recur. Cystectomy with suture closure has been the most effective procedure until now. Sclerotherapy is a new in-office procedure to dissolve the cyst which preserves ovarian function better than cystectomy. Sclerotherapy can help avoid surgery.
What are the stages of endometriosis?
There are four stages of endometriosis. Stage I is referred to as minimal endometriosis because there are not a lot of implants in the pelvis. Stage II is called mild endometriosis and there is more disease. Stage III, or moderate endometriosis, is characterized by even more pain and pelvic organs being affected. Severe endometriosis means stage IV disease and is the most difficult to treat.
What causes endometriosis?
Scientists have not identified the cause of endometriosis so different theories exist. Shedding from the endometrium is a natural part of your period. But not all cells flow out the cervix. During this process, endometrial cells also flow through your fallopian tubes and settle in the pelvic area. Normally the immune system should clean these out. Because of a possible failure of immune system function, the endometrial cells may attach to the tissues in the pelvis. Cyclic bleeding in endometriosis then causes worsening cramps due to inflammation of the surrounding tissue.
Another theory of endometriosis is preprogrammed cell transformation. Some researchers feel the menstrual fluid induces this cell transformation.
Endometriosis tends to run in families, which supports a potential genetic link.
Endometriosis is stimulated by cyclic ovarian estrogen and progesterone production, so symptoms generally subside after menopause. HRT (estrogen with progesterone) for menopause may result in pain.
How many women get endometriosis?
The generally quoted occurrence of endometriosis is 10-15% of women. Endometriosis is more common in caucasian women than other ethnic groups. The majority of women with endometriosis, about 90%, have stage I or II disease. Stage III and IV are less common but usually associated with more pain and faster recurrence.
Is endometriosis cancerous?
Endometriosis itself is not cancer. The incidence of endometrial cancer in women, who have had endometriosis, even if taking estrogen only after a hysterectomy, does not appear very high. There are reports of endometrial cancer arising in endometriosis, so it is possible, but this does not appear to be a contraindication to estrogen for moderate to severe menopausal symptom relief.
What are the signs and symptoms of endometriosis?
The most common symptoms of endometriosis we see at the Advanced Women’s Institute include:
- Worsening menstrual cramps
- Increased days of cramping in the cycle
- New painful intercourse
- Cyclic bowel and/or urinary pain
- Nonspecific bowel and/or urinary pain
- Lower back pain
- Pelvic pressure
What is the best treatment option for endometriosis?
There are two main choices for managing endometriosis, medical or surgical, and both have their merits. Options for medical management include:
- Oral contraceptives (OCs): Generally the first recommendation, especially for younger women. OCs reduce menstrual cramps and flow. Side effects, complications, failure to control pain or return of symptoms may occur. It is possible to give OC’s continuously to extend the interval between periods, thus decreasing periods to 4 or less each year. It doesn’t work for every woman, but is worth a try.
- Progestin IUD: An IUD that releases progestin can reduce or stop the period which help menstrual pain of endometriosis. They are not as effective for non-menstrual pain or pain with intercourse.
- Pain medication: Non-Steroidal Anti-Inflammatory drugs such as ibuprofen can help cramps. This is also a first line treatment and is frequently combined with OCs. Narcotic pain medication can also be used but there is concern about the risk of opioid addiction.
- Progestins: Progestins bind inside the ovary to reduce estrogen production and prevent ovulation. There are oral and injectable(Depo) formulas. Side effects include depression symptoms and abnormal bleeding. Progestins are relatively inexpensive.
- GNRHa (gonadotropin releasing hormone agonist): A class of compounds that selectively stop the pituitary gland from stimulating the ovaries. They are highly effective. The estrogen levels can get so low some women develop hot flashes and night sweats common to menopause. They are also costly.
- GNRH antagonists: They lower estrogen like the agonist, only faster. The side effect profile and patient tolerance is similar to the GNRHa.
There are a variety of medicines available, each with their own side effects. Dr. Moore and the team will discuss each option with you in detail. It should be kept in mind that drug treatment does not cure endometriosis, but continuous use of your medication can help you manage your symptoms effectively. For more permanent solutions, you may opt for a surgical solution, such as:
- Sclerotherapy for endometrioma: This is an in-office procedure to eliminate the endometriosis inside the cyst. The endometrioma cyst disappears. Sclerotherapy can help reduce pain and avoid surgery. It also is less damaging than cystectomy.
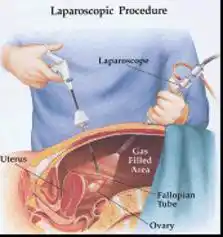
- Laparoscopy: This requires small incisions in the abdomen so a scope can be inserted through the belly button to diagnose and treat endometriosis. If endometriosis is identified at the time of diagnostic laparoscopy, an operative laparoscopy can then be performed to remove the endometrial tissue implants. This requires additional small incisions for the placement of graspers, scissors, and other instruments to remove the implants. The procedure is done as an outpatient and return to work is expected in approximately 2 weeks or less.
- Open Abdominal Surgery for Endometriosis: This procedure is accomplished using a 4-6 inch open abdominal incision to perform the operation. However, laparoscopy represents a less invasive, less painful approach to endometriosis, and is preferable.
There are two surgical solutions, conservative reproductive surgery and permanent hysterectomy surgery.
- Conservative: Endometriosis is treated without removal of organs. Excisional therapy has been shown to be more effective for pain than ablative therapy. We will make sure you go to the right surgeon for you.
- Permanent: Hysterectomy is sometimes the most effective way to help the pain of endometriosis. We will discuss all conservative options as long as it is important to avoid this permanent solution.
What about a natural remedy or diet?
Medical and surgical management have been studied scientifically. Some other ways to help manage endometriosis pain include:
- Heating pad, hot bath, Epsom salt bath can help pain temporarily
- Acupuncture, studies indicate it may help relieve pain temporarily but not long term
- Massage Therapy and self-massage studies indicate temporary but not sustained pain relief
- Rieki is touted for pain relief but lacks scientific support
- Naturopathic medicine is not proven but would not harm, may be costly
- Chinese herbs similarly may help but are not proven and cost may also be an issue
- Herbs such as Tumeric, Pine Bark, Chamomile, Peppermint, Willow Bark, Vitex(Chaste Berry) and Ashwagandha have been reported to help pain but are still controversial
It may be possible to manage some symptoms with various alternative methods. Although controversial, it does not hurt to try them. Cost may be the only issue.